Fraud, Waste, and Abuse: Understanding the Distinctions
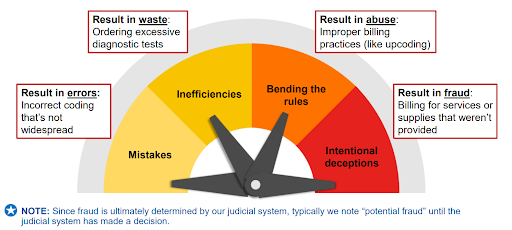
Fraud occurs when an individual intentionally deceives, conceals, or misrepresents information to acquire money or property from a healthcare benefit program.
Waste involves the excessive use of services or other practices that lead to unnecessary costs for any healthcare benefit program, either directly or indirectly.
Abuse refers to actions by healthcare providers or suppliers that cause unnecessary costs to any healthcare benefit program, whether through direct or indirect means.
Level Of Intent
NOTE: Given that fraud is ultimately determined by our judicial system, it is common practice to refer to instances as “potential fraud” until a decision has been reached by the judicial system.
Safeguarding Patients
Our commitment to prioritizing patient welfare includes:
- Endorsing innovative strategies
- Safeguarding the integrity of Medicare Trust Funds
- Preserving the public funds that support Medicaid Programs
- Enhancing program supervision and integrity
- Implementing exclusions for providers with a history of fraudulent activities
- Enforcing regulations to prevent provider reimbursement for undocumented services
Examples of Potential Fraudulent Activities
- Billing Medicare or Medicaid for services or equipment never received or returned
- Providers billing for services that are logistically impossible
- Manipulating documentation to inflate payments
- Misrepresentation of dates, service descriptions, or patient identities
- Misleading tactics by companies to enroll individuals in Medicare health or drug plans using false information
- Unauthorized use of Medicare or Medicaid cards by third parties
Anyone Can Commit Fraud
Fraud can be perpetrated by a wide range of individuals and entities. This includes medical professionals such as doctors and pharmacists, as well as other healthcare providers and their staff. Additionally, those involved in supplying durable medical equipment (DME), operating hospitals, pharmacies, home health organizations, ambulance services, and billing companies can also engage in fraudulent activities.
Furthermore, individuals who have Medicare and/or Medicaid coverage, or those who have illegally obtained their identities, are capable of committing fraud. Even telemarketing companies and health plans can be involved in fraudulent schemes.
Improper Payments
- Should not have occurred
- Were disbursed in inaccurate amounts
- Resulted from fraudulent activities
NOTE: The majority of improper payments stem from unintentional errors such as data entry mistakes or inefficiencies.
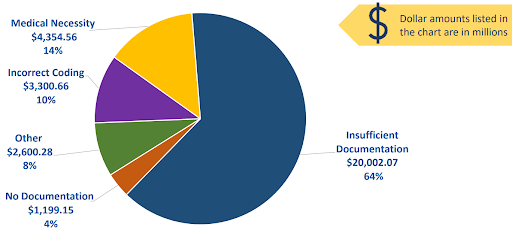
Causes Frequently Leading to Improper Payments
Organizations & Strategies to Detect & Prevent Fraud & Abuse
COVID-19 Fraudulent Schemes
Stay cautious if you encounter:
- Being asked to pay out-of-pocket for a vaccine.
- Requests for your Medicare Number in exchange for a vaccine, booster, or free COVID-19 test.
Remember to:
- Safeguard your Medicare card as you would your credit card.
- Review Medicare claims summary forms for any inaccuracies.
- Immediately end the call if someone requests your Medicare Number.
Preventing Fraud in Medicare Health & Drug Plans
Contact Information for Concerns:
1-800-MEDICARE: (1-800-633-4227)
TTY: 1-877-486-2048
Instances of Concerns:
- The plan is to provide complimentary meals at a promotional event.
- I received an unsolicited email lacking an “opt-out” option.
- A representative attempted to discuss their plan with me in a hospital patient room.
- A plan representative visited my residence without invitation and encouraged enrollment.
- The plan is offering financial incentives for enrollment.
- I am receiving calls and text messages from a plan without my consent.
Common Fraud: Genetic Testing and Orthodontic Braces
“I’m wary of individuals who provide “free” genetic testing or medical equipment and then ask for my Medicare Number.”
“I refuse to accept genetic testing kits or orthotic braces delivered by mail; instead, I send them back to the sender.”
“I maintain a record of all encounters.”
Protect Yourself:
Contact the HHS-OIG Hotline at 1-800-HHS-TIPS (1-800-447-8477) or visit OIG.HHS.gov/fraud/hotline.
Telemarketing & Fraud: Durable Medical Equipment (DME)
Potential DME Scams:
- Unsolicited calls or visits claiming to represent Medicare.
- Employment of phone or door-to-door selling tactics.
- Requests for your Medicare Number.
The Competitive Bidding Program (CBP)
Suppliers engage in competition to secure contracts with Medicare. Serves as a crucial mechanism to:
- Establish payment rates for Durable Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS) based on market dynamics.
- Reduce expenses for Medicare beneficiaries and taxpayers.
- Restrict instances of fraud, waste, and abuse within the Medicare system.
Durable Medicare Equipment Prosthetics, Orthotics, & Supplies (DMEPOS) Competitive Bidding Program (CBP): Round 2021
- Quality – Quality assurance to ensure Medicare beneficiaries receive high-quality products.
- Protection – Protection measures to curb fraud and abuse within the Medicare system.
- Savings – Financial savings benefit taxpayers.
- Efficiency – Operational efficiency through the establishment of a Single Payment Amount (SPA) by Medicare.
Medicare beneficiaries residing in or traveling to Competitive Bidding Areas (CBAs) must utilize an approved contract supplier for Medicare coverage of certain Over-the-Counter (OTS) back or knee braces.
Quality of Care Concerns
Your Beneficiary and Family-Centered Care-Quality Improvement Organization (BFCC-QIO) can address:
- Medication errors.
- Changes in the condition that are not promptly addressed.
- Premature hospital discharges.
- Incomplete discharge instructions and/or arrangements.
Addressing Different Aspects of Fraud, Waste, and Abuse,
CMS implements various measures:
- Stringent screenings for healthcare providers and suppliers.
- Temporary enrollment halts in high-risk regions.
- Suspension or expulsion from all Medicaid Programs and Children’s Health Insurance Programs for providers and suppliers who lose their Medicare billing privileges.
- Temporary cessation of Medicare payments when credible fraud allegations arise.
- Outreach and educational initiatives to meet program goals.
- Collaboration with both private and public health payers and other stakeholders to identify and prevent fraudulent activities in the healthcare system.
The Center for Program Integrity (CPI) at CMS employs several strategies:
- Provider enrollment oversight.
- Data analysis.
- Medical reviews and audits.
- Collaboration with state authorities.
Program Integrity Contractors employed by CMS include:
- Unified Program Integrity Contractors (UPIC).
- Plan Program Integrity Medicare Drug Integrity Contractor (PPI MEDIC).
- Recovery Audit Program.
- Investigations carried out by Medicare Drug Integrity Contractor (I-MEDIC).
Medicare and Medicaid (Medi-Medi) Data Matching Initiative
- Foster collaboration among State Medical Assistance (Medicaid) offices
- Undertake data analyses and investigations collaboratively
- Emphasize voluntary participation by states
- Separate tasks under the UPIC contracts ensure focused efforts
Fraud, Waste, and Abuse Prevention Programs
Mission: Mitigate improper Medicare payments through:
- Detection and retrieval of overpayments
- Identification of underpayments
- Implementation of preventive measures against future payment inaccuracies
State programs, including Medicaid Recovery Audit Contractor (RAC) initiatives:
- Detect and rectify overpayments and underpayments
- Coordinate with federal and state auditors for a streamlined effort
Medicare Drug Integrity Contractors (MEDICs)
Key responsibilities comprise:
- Investigating potential fraud, waste, and abuse within Medicare plans
- Addressing complaints alleging Medicare fraud
- Referring potential fraud cases to law enforcement
- Proactive measures such as data analysis, identifying vulnerabilities, and conducting audits
CMS Administrative Actions
Actions taken when fraud is suspected include:
- Automatic payment denials
- Payment suspensions
- Prepayment edits
- Billing privilege revocations
- Post-payment reviews
- Referrals to law enforcement agencies
Law Enforcement & Judicial System Involvement
Actions encompass:
- Exclusion of providers/companies from programs
- Limiting billing privileges
- Imposing fines
- Legal actions, including arrests and convictions
- Negotiating Corporate Integrity Agreements
Health Care Fraud & Abuse Control (HCFAC) Program
- Jointly overseen by the U.S. Attorney General and the Secretary of the Department of Health & Human Services
- Facilitates coordination among federal, state, and local law enforcement for combating healthcare fraud and abuse
- Annual reporting on program efforts, which include various initiatives like Strike Force Teams and Prevention Partnerships
Medicare Fraud Strike Force Teams
- Strategically placed in areas with high fraud activities
- Utilize advanced data analytics to identify suspicious billing patterns
- Coordinate national enforcement actions
Health Care Prevention & Enforcement Action Team (HEAT)
- Aims to prevent fraud, waste, and abuse in Medicare and Medicaid Programs
- Targets inappropriate opioid prescriptions and promotes best practices
- Enhances collaboration between HHS and DOJ
Health Care Fraud Prevention Partnership (HFPP)
- Enhances fraud detection and prevention through:
- Data exchange between public and private sectors
- Utilization of analytic tools against the provided data sets
- Facilitating the sharing of successful anti-fraud practices
Major Case Coordination (MCC)
- Enables collaboration among policy experts, law enforcement, clinicians, and fraud investigators
- Results in numerous reviews, law enforcement referrals, and nationwide enforcement actions
Provider Education
- Aids in addressing vulnerabilities by:
- Ensuring proper documentation
- Reducing inappropriate claims
- Safeguarding patient and provider identity
- Cultivating a culture of compliance within the provider community
How People with Medicare & Medicaid Can Fight Fraud
Consequences of Sharing Your Health Care Card or Number
- Inaccurate Medical Records – Sharing your health care card or number can lead to errors in your medical records.
- Health Care Fraud Charges – Sharing your information may result in being charged with health care fraud.
- Loss of Benefits – Sharing your health care details could result in losing your benefits.
- Enrollment in Lock-In Programs – Medicaid recipients risk being enrolled in lock-in programs if their information is shared.
Senior Medicare Patrol (SMP)
- Education on Fraud Prevention – SMP educates individuals with Medicare about how to prevent, identify, and report healthcare fraud.
- Volunteer Opportunities – SMP offers opportunities for volunteers to represent their communities in combating fraud.
- Complaint Resolution – SMP hears and addresses complaints from individuals with Medicare.
Note: It’s important to note that SMP operates actively across all states, the District of Columbia, Puerto Rico, U.S. Virgin Islands, and Guam.
Experience The Convenience And Security Of The Electronic Medicare Summary Notice (EMSN) By Enrolling Today
Receive monthly email notifications when your MSNs are ready in your Medicare account, eliminating the three-month waiting period. Enjoy the ease of accessing your MSNs electronically, without the need for mailed paper copies.
Enhance your Medicare account on Medicare.gov with these valuable features:
- Print an official copy of your Medicare card instantly.
- Access and securely share your electronic health information.
- Conveniently pay your Original Medicare premiums online.
- Easily view your Original Medicare claims.
- Explore and compare plans available in your area.
- Compile a comprehensive list of your prescribed medications.
- Receive assistance through live chat support.
Stay informed and empowered with the Explanation of Benefits (EOB) provided by Medicare Advantage Plans and Medicare drug plans, offering transparent and timely details about your medical and/or drug claims.
Empower yourself against Medicare fraud with the “4 Rs” strategy:
- Record all appointments and services accurately.
- Review services provided to ensure accuracy.
- Report any suspected fraudulent activities promptly.
- Remember to safeguard your personal information (“guard your card”).
For additional guidance on combating Medicare fraud, visit Medicare.gov/publications and review “4 Rs for Fighting Medicare Fraud” (Medicare Product No. 11610).
If you encounter any issues or suspect fraud, contact Medicare promptly:
Call 1-800-MEDICARE (1-800-633-4227) to lodge a complaint or report fraud. Ensure you have relevant information available, including the provider’s name and any identifying numbers, details of the item or service, the date and payment amount, the date on your MSN, and your name and Medicare Number.
Your vigilance against fraud can be rewarded:
- If the fraud you report is substantiated, and formally referred to the U.S. Department of Health & Human Services (HHS) Office of the Inspector General (OIG).
- Provided you are not classified as an “excluded individual” and the reported individual or organization is not already under investigation by law enforcement.
- Your report directly contributes to the recovery of at least $100 of Medicare funds.
In Summary
Preventing fraud and abuse in Medicare and Medicaid requires a multi-faceted approach that encompasses understanding the distinctions between fraud, waste, and abuse, as well as implementing rigorous safeguards and detection mechanisms. From endorsing innovative strategies to enforcing regulations and implementing exclusion measures, various initiatives are in place to protect patient welfare and the integrity of healthcare benefit programs.
Vigilance is key for both providers and beneficiaries, with proactive measures such as reporting suspicious activities and safeguarding personal information. Through collaboration between regulatory bodies, law enforcement agencies, and vigilant individuals, we can strive to mitigate improper payments, uphold program integrity, and combat fraudulent schemes effectively.
DISCLAIMER: Please verify the information provided here with the primary source to ensure accuracy. We strive to present information correctly. It is advisable to confirm details directly from the primary source for accuracy and reliability