Medicare guarantees rights and protection for anyone receiving Medicare services, ensuring they can access necessary medical care. This law ensures Americans receive the healthcare they need without discrimination and protects their personal health information. It’s crucial for individuals to understand their Medicare rights to make informed decisions about their medical care and avoid any mistreatment or privacy breaches.
Medicare Rights
Your healthcare has rights and important protection. These are the regulations that make you safe and well-covered in your medical appointments. Furthermore, it guarantees that patients receive the right healthcare services as required by the law. It also protects you from getting mistreated unfairly or unethically, which may have a negative effect on your health. Also, it ensures that your privacy is considered, and your applicable healthcare information is kept private. It’s crucial to have these rights that give you the confidence and sense of security to seek medical help.
Your Rights in Original Medicare
1. Protection from Unfair Treatment & Discrimination
You have the right to be treated well and respectfully, protected from unfair treatment, and receive Medicare information that you can easily understand and use. These rights ensure you are treated fairly and can access the healthcare services you need.
2. Information
You have the right to keep your personal and health information private and receive healthcare information that is easy for you to understand. This helps you make informed decisions about your healthcare.
3. Access to Care
You have the right to see doctors, and specialists, and go to hospitals for necessary medical care. You should also be able to understand your treatment options, participate in decisions about your care, and receive Medicare information in a language you understand. Additionally, you can get Medicare-covered services during emergencies, wherever and whenever you need them.
4. Grievances
You can file complaints (also known as grievances) if you feel something is wrong about:
- A doctor, hospital, or provider
- The quality of the care you experience
- Health and Drug plan
- Dialysis or Kidney transplant care
- Durable Medical Equipment (DME)
You can also file a complaint about your concerns on the quality of care you’re getting:
- For Original Medicare, contact the Beneficiary and Family Centered Care-Quality Improvement Organization (BFCC-QIO) serving your area.
- For a Medicare Advantage Plan or Medicare prescription drug plan, contact the BFCC-QIO, your plan, or both if needed.
- If you are diagnosed with End-Stage Renal Disease (ESRD), contact the ESRD network in your state for assistance.
The table below shows your Beneficiary & Family Centered Care-Quality Improvement Organizations (BFCC-QIO) Service Areas:
QIO | REGION |
Area 1: KEPRO | CT, ME, MA, NH, RI, VT |
Area 2: Livanta BFCC-QIO Program | NJ, NY, PR, VI |
Area 3: Livanta BFCC-QIO Program | DE, DC, MD, PA, VA, WV |
Area 4: KEPRO | AL, FL, GA, KY, MS, NC, SC, TN |
Area 5: Livanta BFCC-QIO Program | IL, IN, MI, MN, OH, WI |
Area 6: KEPRO | AR, LA, NM, OK, TX |
Area 7: Livanta BFCC-QIO Program | IA, KS, MO, NE |
Area 8: KEPRO | CO, MT, ND, SD, UT, WY |
Area 9: Livanta BFCC-QIO Program | AZ, CA, HI, NV, Pacific Islands |
Area 10: KEPRO | AK, ID, OR, WA |
Your Rights in a Medicare Advantage Plan or Other Medicare Health Plans
You have the right to pick doctors and healthcare providers that are part of your plan’s group. Your doctor should give you a treatment plan that explains your care. You can also ask how your doctors are paid and get information about what your plan covers. If you disagree with a coverage decision, you can request an appeal. And if you have any problems or concerns, you can file a complaint with your plan.
Your Rights with Medicare Drug Coverage
You can ask your plan to decide if they will cover something or appeal if you disagree with their decision. If you have a problem with your plan, you can file a complaint, also known as a grievance. Your health and drug information should be kept private and confidential.
Appeal Rights
If you don’t agree with a decision Medicare or your Medicare Plan has made about what they will cover or pay for, you can take action by making an appeal to try to change their decision.
Discover your rights to challenge decisions about your Medicare coverage, no matter how you receive it. Learn how to challenge coverage or payment decisions and where to get help with the appeals process. Find out the steps and timing for appealing decisions with Original Medicare, Medicare Advantage Plans, and Medicare drug coverage. Explore the faster process for appealing decisions with Original Medicare, Medicare Advantage Plans, and Medicare drug coverage, including the steps and timing.
Appeal Rights in Original Medicare
You can ask for an appeal if Medicare doesn’t cover something you think it should, if a payment is denied that you believe should have been covered, or if you disagree with a Medicare coverage or payment decision. This helps you get a review of decisions you believe are unfair or incorrect.
Expedited or Fast Appeals in Original Medicare
You can request an expedited appeal if you feel you are being discharged too early from a hospital stay covered by Medicare or if your services from a Skilled Nursing Facility (SNF), Home Health Agency (HHA), Comprehensive Outpatient Rehabilitation Facility (CORF), or Hospice ended too soon. This allows for a faster review if you believe your care is being cut short unfairly.
You should call the BFCC-QIO in your region to help you out and for clarification.
NOTE: You will get important notices or messages about your rights within 2 days prior to your hospital admission (inpatient). You will be notified for your NOMNC (Non-Coverage) at least 2 days before your covered services will end.
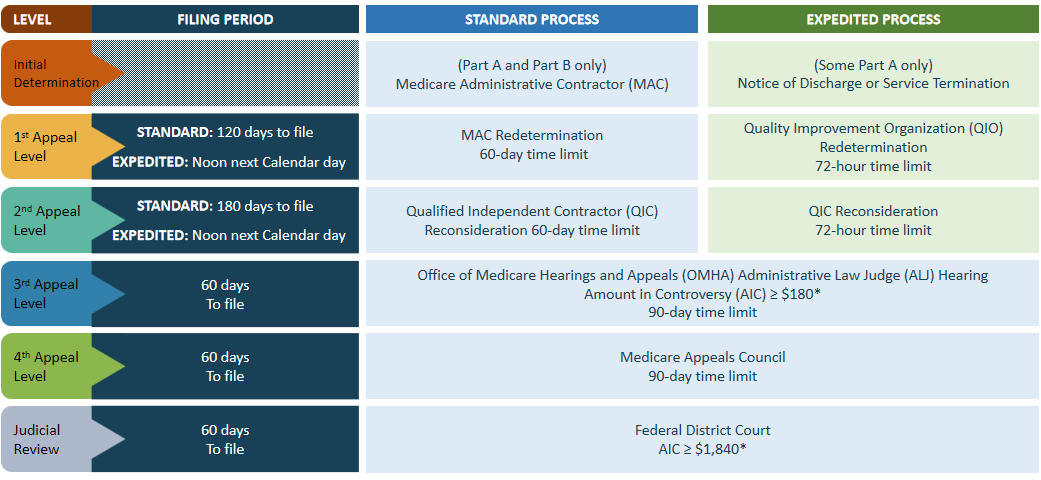
Part A & Part B (Original Medicare) Appeals Process
Below shows a table that consists of the process and timeframe in filing an appeal. It shows the difference between Standard Process and Expedited Process.
NOTE: The time to file your appeal starts from the day you receive the previous decision or determination. The amount of money needed to file an appeal for an ALJ hearing or in Federal District Court changes every year based on the medical care component of the consumer price index. The chart below shows the specific amounts for the year 2024.
Appeal Rights in a Medicare Plan or Other Health Plans
You can ask for an appeal if you disagree with your plan’s decision, and you have the right to access your file by contacting your plan, presenting evidence to support your case, and requesting a fast appeal if needed. This helps you address any disagreements or concerns you have about your healthcare coverage quickly and fairly.
Expedited or Fast Appeals in a Medicare Plan or Other Health Plans
You can request an expedited appeal if you feel you are being discharged too early from a hospital stay covered by Medicare or if your services from a Skilled Nursing Facility (SNF), Home Health Agency (HHA), Comprehensive Outpatient Rehabilitation Facility (CORF), or Hospice ended too soon. This allows for a faster review if you believe your care is being cut short unfairly.
NOTE: You will get important notices or messages about your rights within 2 days prior to your hospital admission (inpatient). You will be notified for your NOMNC (Non-Coverage) at least 2 days before your covered services will end.
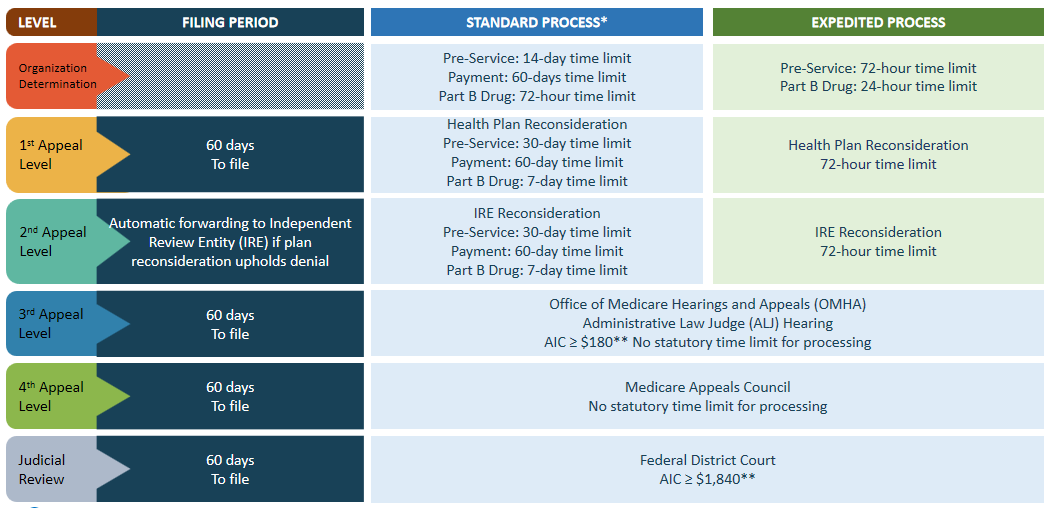
Part C (Medicare Advantage) Appeals Process
Below shows a table that consists of the process and timeframe in filing an appeal. It shows the difference between Standard Process and Expedited Process.
NOTE: You can begin the filing process for an appeal once you receive the decision or determination you want to challenge. In 2024, health plans are required to process 95% of clean claims from out-of-network providers within 30 days and all other claims within 60 days. The Administrative Law Judge (ALJ) hearing and Federal District Court requirement is adjusted annually based on the medical care component of the consumer price index, with specific amounts for 2024 outlined in the provided chart.
Appeal Rights with Medicare Drug Coverage (Coverage Determination Request)
The first decision your plan makes about your drug benefits includes determining if a specific drug is covered, confirming if you meet all requirements to receive the drug, setting the cost you need to pay for the drug, and deciding whether to make an exception to a plan rule upon request. This initial decision by your plan affects how you access and pay for medications under your coverage.
The processing time for this decision is 72 hours prior to Standard Process, while for Expedited Process it will take 24 hours.
You, your healthcare provider, or someone you appoint to act on your behalf can make the request for these decisions about your drug benefits.
How to Appoint a Representative?
You can appoint a representative in 3 ways. These are:
- You must fill out the “Appointment of Representative” form
- You should make and submit a written request of your appeal that includes the following information:
- Personal Details (Name, Address, Phone Number, and Medicare Number)
- Include a statement about choosing someone to represent on your behalf (Include the details of your representative – Name, Address, Phone Number, and their professional status or relationship to you such as doctor or family member)
- Create a statement that you authorize your representative to gain access of your personal and identifiable information
- An explanation of why you need representative and to what extent they will assist you.
Submit the request in your Medicare account (Medicare.gov)
Exception Requests
An exception refers to a decision made about your coverage, and there are two types namely Tier Exceptions and Formulary Exceptions. You will need a supporting statement issued by your prescriber in submitting this request. An exception may be valid for the rest of the year.
- Tier Exceptions : If your health plan uses different cost tiers for drugs, they must provide tiering exceptions allowing you to access a non-preferred drug at a lower cost. This allows you to pay less for certain medications based on their tiering structure and available alternatives for your condition.
The plan may apply certain limitations, such as allowing tiering exceptions for brand name drugs to the lowest cost sharing associated with brand name alternatives, tiering exceptions for biological products to the lowest cost sharing associated with biological alternatives, and tiering exceptions for non-preferred generic drugs to the lowest cost sharing associated with either brand or generic alternatives. These limitations determine how tiering exceptions apply based on the type of drug and its alternatives within the plan’s structure.
NOTE: Insurance plans are not obliged to provide tiering exceptions for brand name drugs or biological products if lower-cost alternatives, such as generic or authorized generic drugs, are available at a different cost-sharing level.
- Formulary Exceptions : The plan is required to approve a formulary exception if all available formulary alternatives are not as effective or if the alternative drug could cause adverse effects. Additionally, an exception to a coverage rule must be granted if the drug has been ineffective in treating your condition or if it has caused harm or is likely to cause harm.
Note: When you ask for an exception to your insurance plan’s drug coverage, your doctor or prescriber must provide a statement to the plan. This statement explains why you specifically need the requested drug.
Requesting Part D Appeals
If your request for coverage determination, exception, or coverage limitation is denied, you have the right to request a redetermination. Plans must accept fast-track requests made verbally, and the request must be made within 60 days from the date of the coverage decision. This allows for a prompt review of your request.
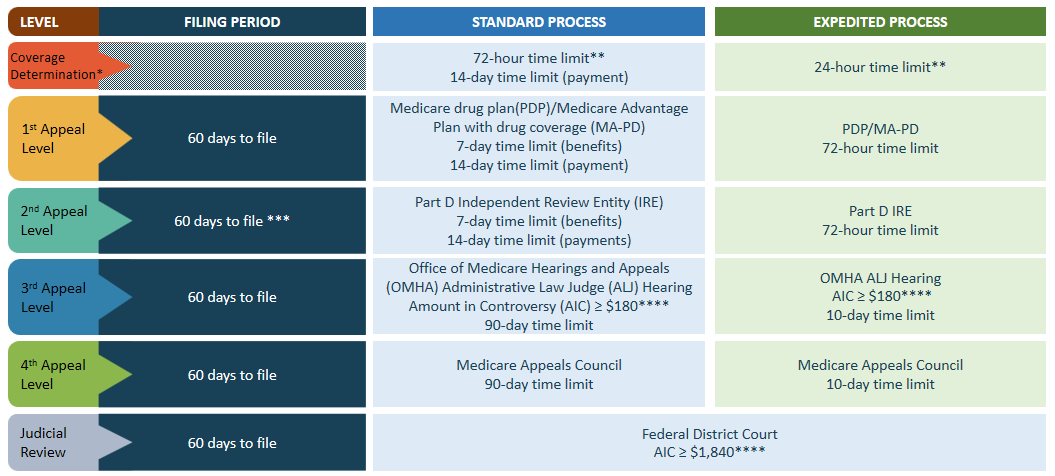
Part D (Drug) Appeals Process
Below is a table that consists of the process and timeframe for filing an appeal. It shows the difference between the Standard Process and the Expedited Process.
NOTE: A request for a coverage determination can include asking for a tiering exception or a formulary exception. This request can be made by the enrollee, their appointed representative, or their healthcare provider. The timeline for processing the request typically starts when the plan sponsor receives it, though for exception requests, it begins upon receipt of the physician’s supporting statement. If a plan sponsor upholds a decision that an enrollee is at-risk per 42 CFR § 423.153(f) during a redetermination, the case must be automatically forwarded to the Part D Independent Review Entity (IRE). Additionally, the AIC (Amount in Controversy) requirement for an Administrative Law Judge (ALJ) hearing and Federal District Court is adjusted annually based on the medical care component of the consumer price index, with specific amounts for calendar year 2024 detailed in the chart.
Your Rights in Certain Benefits
1. Right to Hospital Care
You have the right to receive medically necessary hospital care covered by Medicare to diagnose and treat illnesses or injuries, as well as to receive follow-up care to ensure you recover well. This means Medicare will help cover essential hospital services to help you get better and stay healthy.
NOTE: You will get important notices or messages about your rights within 2 days prior to your hospital admission (inpatient) and no more than 2 days before your discharge date. You will be notified for your Medicare Outpatient Observation Notice (MOON) if you avail this service as an outpatient for more than 24 hours.
2. Rights in a Skilled Nursing Facility (SNF)
You have the right to see your own doctor for medical care, handle your own money, make a complaint if something isn’t right, spend time with visitors when it’s convenient for you, and have family members and legal guardians involved in your care decisions. These rights ensure you have control over your healthcare and personal choices.
3. Rights in Home Health and Hospice Care
Before you start receiving care, you will receive a written document outlining your rights and responsibilities. This includes your right to appeal decisions, select your care agency, have your property respected, receive and review your care plan, and have a family member or guardian make decisions for you if you are unable to do so. This information ensures that you understand what you are entitled to and how you can participate in your care.
4. Rights in Other Settings – Comprehensive Outpatient Rehabilitation Facility (CORF)
In a CORF (Comprehensive Outpatient Rehabilitation Facility) setting, your provider will explain your treatment plan for rehabilitation. If your provider offers non-therapy services at the CORF, these services must be related to your rehabilitation treatment plan. Medicare does not have a yearly payment limit for medically necessary physical therapy, speech-language pathology services together, or occupational therapy services. This means you can receive the therapy you need without worrying about payment limits for these services within a calendar year.
Medicare Privacy Practices and Additional Protection
The Notice of Privacy Practices explains how Medicare uses and shares your personal medical information and describes your rights and how to use them. You can find this information every year in the “Medicare & You” handbook and on Medicare.gov.
For more details, you can call 1-800-MEDICARE (1-800-633-4227) (TTY: 1-877-486-2048). This helps you understand how Medicare protects your privacy and how you can access your rights.
Personal Medical Information Privacy Rights
You have the right to request a copy of the information Medicare has about you, a list of who has accessed your information from Medicare, a notification letter if there’s a privacy risk, and a printed copy of the “Notice of Privacy Practices.” These options allow you to stay informed and have control over your personal health information.
You can request that Medicare communicate with you in a different way or at a different place that works better for you. You also have the right to limit how your information is used and shared for paying your medical claims. This helps you manage how Medicare handles your personal information.
And, you can ask Medicare to update your information if you believe it’s incorrect or incomplete. Additionally, you can speak to a Customer Service Representative if you have questions about Medicare’s privacy notice. This ensures that your information is accurate and that you understand how Medicare protects your privacy.
How to Report if Your Privacy Rights are Violated?
Medicare, Medicaid, and military/veterans health care programs are protected under the Health Insurance Portability and Accountability Act (HIPAA). You can file a complaint in writing by email, mail, or through the Office of Civil Rights (OCR) Complaint Portal if you have privacy concerns. Filing a complaint will not impact your Medicare benefits in any way. This ensures that your privacy rights are upheld without affecting your health care coverage.
Reporting via email? You can send it here: OCRComplaint@hhs.gov
Reporting via portal? You can submit it here: ocrportal.HHS.gov
If you will send it via mail, here are the details for the address:
Centralized Case Management Operations
U.S. Department of Health & Human Services
200 Independence Avenue, S.W.
Room 509F HHH Bldg.
Washington, D.C. 20201
What are Advance Directives?
Advance Directives are legal documents that outline your wishes for medical decisions if you are unable to make them yourself. They come in two main types: a Health Care Proxy (durable power of attorney), which designates someone to make decisions on your behalf, and a Living Will, which specifies your preferences for medical treatment and end-of-life care. These documents ensure that your wishes are followed when you cannot communicate your decisions.
Who is in charge of Reviewing and Resolving Complaints?
The Medicare Beneficiary Ombudsman ensures that information is accessible to help you make informed healthcare decisions and understand your Medicare rights. The Competitive Acquisition Ombudsman assists in resolving complaints related to specific durable medical equipment (DME), prosthetics, orthotics, and supplies under Medicare. These resources are here to support you and address any concerns you may have about your Medicare coverage.
In Summary
Medicare ensures individuals receive the healthcare they need without discrimination and protects their personal health information. The Medicare Beneficiary Ombudsman and Competitive Acquisition Ombudsman assist in resolving complaints to ensure you receive fair treatment and access necessary services under Medicare.
This discusses Medicare rights and protections, ensuring individuals receive necessary healthcare without discrimination. It covers key rights, including access to healthcare, privacy protection, and the ability to file complaints. Medicare beneficiaries have the right to choose their doctors, understand their treatment plans, and file appeals or complaints if needed. Additionally, there are specific rights related to hospital care, skilled nursing facilities, and home health and hospice care.
Knowing and utilizing these rights is essential for navigating the Medicare system effectively and receiving quality care. It’s important to know your Medicare rights to make informed decisions about care and avoid mistreatment or privacy breaches.
DISCLAIMER: Please verify the information provided here with the primary source to ensure accuracy. We strive to present information correctly. It is advisable to confirm details directly from the primary source for accuracy and reliability.