What Are Special Needs Plans?
A Special Needs Plan (SNP) is a type of healthcare plan for people who have special needs. This plan is a part of Medicare, which is a government program that helps people pay for medical care. The SNP is like a special team that gives personalized care to people who need it. These people might live in institutions, have both Medicare and Medicaid, or have serious health conditions.
The way Special Needs Plans (SNPs) get paid is similar to how other Medicare plans get paid. The government gives money every month to the organization that runs the SNP for each person in the plan. This money is supposed to pay for the medical care that the person needs.
To join an SNP, you need to meet certain requirements based on your health needs. The SNP will check if you qualify. You can join by contacting us at 1-888-559-0103 and talk to one of our agents to help you.
This appointment is meant to alleviate any concerns and there is no-cost or obligation to make a change.
Benefits of Special Needs Plans: What You Need to Know
Special Needs Plans (SNP) offer special benefits that go beyond regular Medicare plans. These benefits include:
- Lower or no cost for patients.
- More time is covered for hospital stays.
- Longer coverage for special medical treatments.
- Equal coverage for both physical and mental health.
- Extra check-ups like dental, vision, and hearing tests, as well as screenings for cancer and heart problems.
- Help connecting to community services for money and transportation.
- Programs to help you stay healthy and manage long-term illnesses.
Things You Need to Know About SNPs
What are the payment procedures of SNPs?
Payment procedures for SNPs are similar to how CMS pays other Medicare Advantage (MA) plans. CMS gives money to MA organizations every month in advance, which is known as capitated payments, for each person enrolled. This money covers the costs of Medicare benefits in a specific area.
Do SNPs Focus on Quality?
Yes, just like other Medicare plans, Special Needs Plans have to work on improving the quality of care. They have special programs to help people with their health conditions.
What Happens if Your Health Situation Changes?
If you no longer meet the special health needs criteria, you’ll get a chance to switch plans. If you’re in a special health plan but don’t qualify anymore because you don’t have the special needs they require, you can still switch plans. The government gives you extra time to pick a new plan during a Special Enrollment Period (SEP). The plan you’re leaving has to tell you that you’re not in it anymore.
Navigating Chronic Conditions: A Guide to Special Needs Plans
What is a Chronic Condition Special Needs Plan?
Chronic Condition Special Needs Plans (C-SNPs) are Special Needs Plans (SNPs) that limit enrollment to individuals with particularly severe or disabling chronic conditions. About two-thirds of Medicare beneficiaries have several chronic conditions, needing coordinated care among various healthcare providers, facilities, and services. C-SNPs are tailored to focus on enrolling Medicare beneficiaries with severe or disabling chronic conditions specifically.
Specific Chronic Conditions Required to Be Eligible for a C-SNP
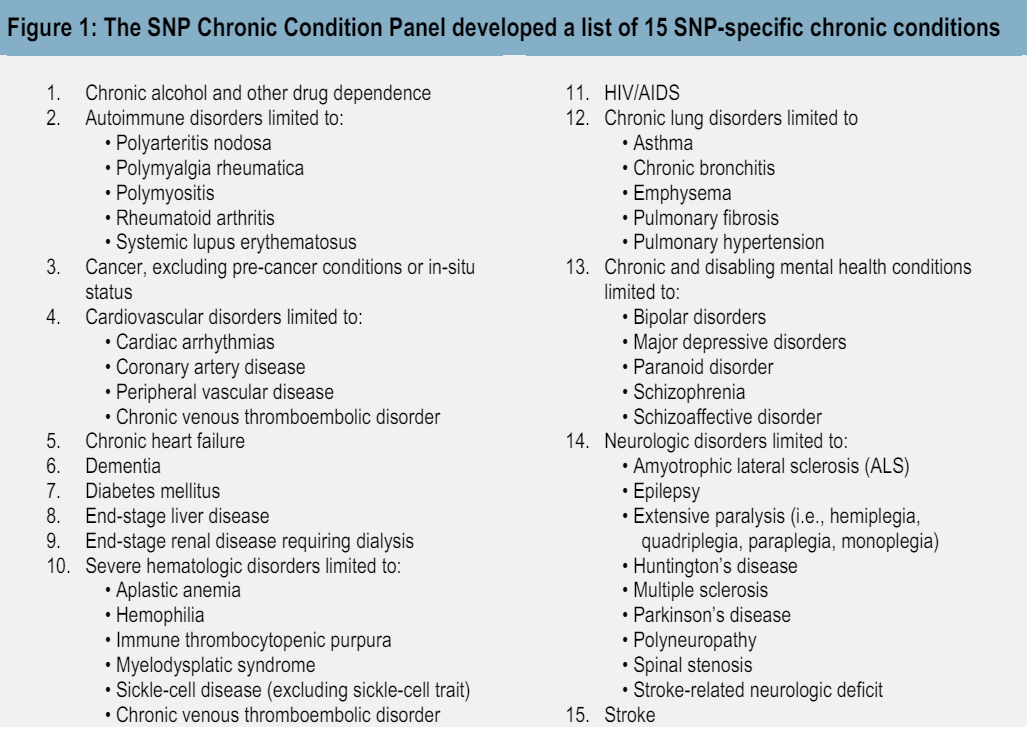
People with special needs who have serious and long-lasting health problems are called individuals with “severe or disabling chronic conditions.” These are conditions that can make life very hard, increase the chances of going to the hospital, and need special care in different areas. CMS has endorsed 15 SNP- specific chronic conditions (refer to Figure 1 below).
How is eligibility for a C-SNP verified?
To see if a special needs person can join a C-SNP, CMS needs the C-SNP to check with their current doctor to make sure they have the right conditions. The C-SNP has to check if the person still qualifies at least once a year.
MA organizations can ask CMS if they can use a tool before enrolling someone to check if they qualify for a certain C-SNP. If a C-SNP uses this tool and enrolls someone based on it, they have to get confirmation from the person’s doctor in the first month. If they can’t confirm it by the end of the first month, the person will be removed from the plan by the end of the second month.
Exploring the Benefits of Dual Eligibility Special Needs Plans (D-SNPs)
What is a Dual Eligible Special Needs Plan?
Dual Eligible Special Needs Plans (D-SNPs) are special health plans for people who qualify for both Medicare and Medicaid.
“Dual eligible” refers to people who get help from both Medicare and Medicaid. This includes those who get all Medicaid benefits and those who only get help with Medicare costs. Whether someone qualifies for dual-eligible coverage depends on their income and what they own.
Uncovering the Medicaid Eligibility Categories
Dual eligible beneficiaries fit into one of seven categories for Medicaid eligibility. Each state may have different rules for deciding who qualifies, leading to differences between states. Here are the main categories:
- QMB only: People with low income and resources who get help from Medicaid for Medicare Part A premiums, Part B premiums, and certain other costs.
- QMB+: Those who meet QMB standards and can get full Medicaid benefits, often by meeting specific standards or spending down extra income.
- SLMB-only: Individuals with slightly higher income who qualify for help with Part B premiums through Medicaid but don’t get other Medicaid benefits.
- SLMB+: Those who meet SLMB standards and also get full Medicaid benefits.
- Qualifying Individual (QI): People with slightly higher income who can get help with Part B premiums through Medicaid.
- Qualified Disabled and Working Individual (QDWI): Those who can get help with Part A premiums through Medicaid and meet certain income and resource criteria.
- Other full benefit dual eligible (FBDE): People who don’t meet QMB or SLMB criteria but can get Medicaid through different groups based on specific circumstances.
Institutional SNPS: What You Need to Know
What is an Institutional Special Needs Plan?
Institutional Special Needs Plans (I-SNPs) are SNPs that limit enrollment to Medicare Advantage (MA) eligible individuals who have required or are anticipated to need services provided in long-term care facilities like skilled nursing facilities (SNFs), nursing facilities (NFs), intermediate care facilities (ICFs) for the developmentally disabled, or inpatient psychiatric facilities for a period of 90 days or more.
If you live in a long-term care facility and qualify for Medicare, you can join institutional special needs plans. If you move to a different long-term care facility, your SNP will help you transition to a new plan if needed. SNPs that serve long-term care facilities need to have certain agreements in place to provide care properly.
Summary
Special Needs Plans (SNPs) offer tailored healthcare options for Medicare beneficiaries with specific needs, such as chronic conditions, dual eligibility, or institutional care requirements. SNPs vary in their eligibility criteria, benefits, and enrollment processes, ensuring individuals receive comprehensive and coordinated care. Whether it’s Chronic Condition SNPs, Dual Eligible SNPs, or Institutional SNPs, CMS sets guidelines to guarantee quality care and accessibility. Understanding the diverse options and requirements of SNPs empowers beneficiaries to make informed decisions about their healthcare coverage.
To gain further insight into Special Needs Plans (SNPs), feel free to reach out to one of our reliable representatives directly at 1-888-559-0103.