What is Medicaid?
Medicaid is a program that assists people with low income to get medical care. It is a collaboration between the federal government and each state. Therefore, each state has its own set of criteria to determine who is eligible for Medicaid and what services it covers.
To be eligible for Medicaid, you must typically have limited income and resources, such as savings or property. Approximately 85.9 million people in the United States are currently covered by Medicaid. It operates in conjunction with Medicare to assist around 12 million individuals who are 65 years old or older, have a disability, or are suffering from severe kidney problems, also known as End-Stage Renal Disease.
If you believe you may qualify for Medicaid, you can contact your state’s Medicaid office to learn more.
Federal Medicaid Administration
The Federal Medicaid Administration has established specific rules that all states in the United States must adhere to when it comes to Medicaid. These rules comprise guidelines on who qualifies for it and which services are eligible for coverage.
The federal government provides funding to every state to aid in the payment of these services. The amount of money allocated to each state is based on the Federal Medical Assistance Percentage (FMAP), which is calculated according to the average income of the residents of each state.
This percentage is subject to change annually and is made public by the U.S. Department of Health & Human Services. Therefore, each state’s share of Medicaid expenditures can vary based on the average income of its residents.
State Medicaid Administration
In the United States, the State Medicaid Administration is responsible for operating its programs. Each state is governed by general rules set by the federal government, but they have the freedom to create and manage their own Medicaid Plan. This plan outlines who is eligible for Medicaid, the types of healthcare services that are covered, and the compensation healthcare providers receive for their services.
The state governments work with the Centers for Medicare and Medicaid Services (CMS) to ensure that their programs run smoothly. States may make changes to their Medicaid plans, such as who qualifies for it, what services are offered, or how much providers are paid, but they must obtain approval from CMS first. As a result, their programs may differ slightly from state to state due to variations in the rules and decisions of each state.
Single State Medicaid Agency
The Single State Medicaid Agency is the primary entity responsible for administering the Medicaid program in each state. This agency is responsible for overseeing all aspects of it, including determining eligibility criteria and the types of services provided. In most cases, this agency is a part of the Department of Health.
If you need assistance applying for Medicaid or have any questions about the program in your state, this is the place to go. The Single State Medicaid Agency ensures that it is functioning efficiently and effectively, providing medical care to those who require it but cannot afford it on their own.
You might find this agency under different names in your area, such as:
- Social Services
- Public Assistance
- Human Services
Eligibility of Medicaid
Understanding who can qualify for Medicaid is important for getting healthcare assistance when needed. To be eligible for Medicaid in your state, certain basic requirements must be met. These include:
- To get Medicaid in your state, you need to live there, fit into a group specified by Medicaid laws (like low-income families or pregnant women), and meet specific financial and other criteria.
- Eligibility groups specified in the federal Medicaid law include:
- Low-income families with children
- Pregnant women
- Individuals with disabilities (blind, etc….)
- Elderly individuals (Age 65 or over)
- Individuals getting Supplemental Security Income (SSI)
- States have the option to broaden eligibility to adults aged 19–64 with low income who are not covered by Medicare Part A or Part B and who are not pregnant.
- In states where Medicaid has been expanded as mentioned earlier, you may be eligible if you meet the income threshold and other non-financial criteria, such as residency and citizenship requirements.
NOTE: Some states provide coverage to adults under special waivers with varying income thresholds.
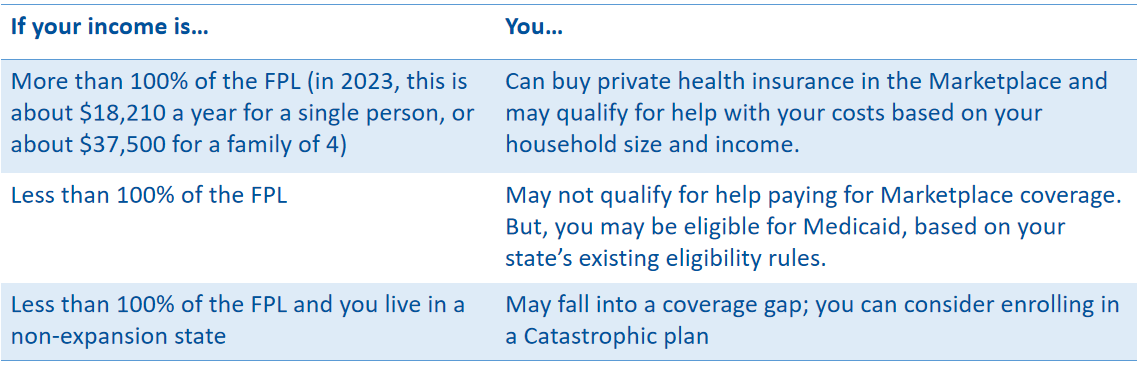
Medicaid eligibility can vary depending on whether a state has expanded its program. You may not qualify for it or a discounted private insurance plan through the Health Insurance Marketplace®. The illustration below shows an example:
For additional details regarding Medicaid expansion, you can visit the website.
What is Modified Adjusted Gross Income (MAGI)?
To determine the eligibility for healthcare benefits and tax credits, federal income tax rules are utilized. These rules help in calculating the total income of a family and the number of individuals living in a household. MAGI-based rules come in handy as they act as a special calculator that helps determine whether a person can avail Medicaid or CHIP, even if they haven’t filed tax returns.
These rules also help in deciding if a person can receive discounts on health insurance via the Marketplace. By using these rules, families can easily know if they are eligible for medical expense assistance.
MAGI, which stands for Modified Adjusted Gross Income, is connected to how much money you pay taxes on. When deciding if you qualify for Medicaid or CHIP, they ignore a bit of your income, like 5% of the Federal Poverty Level.
They look at who you claim on your taxes and who depends on you for support. Things like child support, which aren’t taxed, don’t count. And sometimes, if someone is pregnant, the rules for how many people are in the household might change.
Who Qualifies Based on Modified Adjusted Gross Income (MAGI)?
People who rely on Modified Adjusted Gross Income (MAGI) include:
- Adult group
- Children
- Pregnant Individuals
- Parents and Other Caretaker Relatives
People exempt from MAGI considerations include those who:
- Do not require an income assessment, such as recipients of SSI or federal foster care or adoption support
- Qualify due to age, vision impairment, or disability
- Require extended medical care
- Qualify for assistance with Medicare expenses
- Are categorized as “medically needy”
Single, Streamlined Application Process
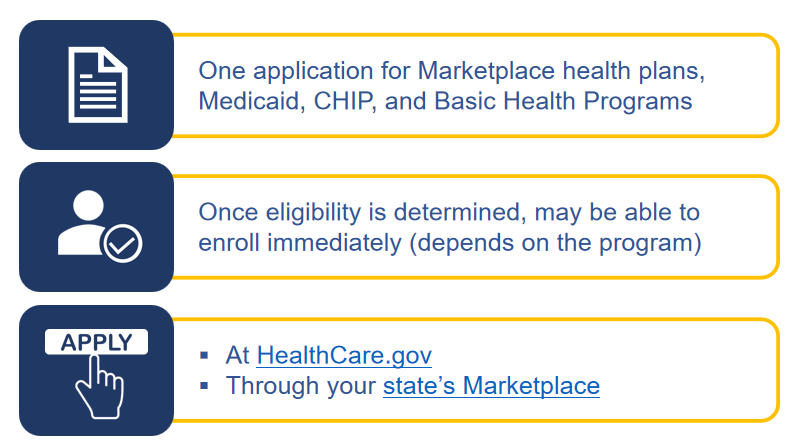
Below is an illustration of the steps of the application process.
Verifying Eligibility with Federal Data Service Hub
Medicaid and CHIP rules make it easier for states, applicants, and Medicaid recipients to apply, sign up, and renew benefits.
- Applicants provide details about their eligibility, such as household composition, state residency, and income. The state checks this information to make sure it’s true. They mainly use reliable electronic sources to do this, unless the law says they need to check something else, like citizenship. States can sometimes take what applicants say as true without needing more proof to decide if they qualify. They can also choose which sources to use for information, but there are some rules they have to follow. After getting data from these sources, states check things like income and where applicants live before asking for more details.
- The Federal Data Services Hub sends information electronically from federal agencies. This includes tax and benefits details from the IRS, Social Security, and the U.S. Department of Homeland Security for confirming non-citizen status. In some states, you might find out if you qualify for benefits right away.
- If you’re eligible for Medicaid, your coverage typically starts on the day you apply or at the beginning of the month you apply. Your state might also cover your benefits for up to 3 months before you apply if you would have qualified during that time. However, your coverage usually ends at the end of the month when you no longer meet the eligibility criteria.
- If you’re enrolled using the simple income-based rules, you only need to renew once every 12 months, unless you tell the agency about a change or they find out something that might affect your eligibility.
- States can choose to give children continuous eligibility for 12 months through Medicaid and CHIP, even if their family’s income or situation changes during that time.
Coverage of Mandatory Medicaid Benefits
These include:
- Staying in the hospital overnight for medical care
- Getting medical care at the hospital without staying overnight
- Health check-ups, tests, and treatments for children under 21
- Getting care in a nursing facility (except for those who qualify based on medical need)
- Receiving medical care at home for people who need nursing facility care
- Visiting a doctor for check-ups and treatments
- Getting medical care at a rural health clinic
- Treatment for addiction with medications
- Family planning services
- Costs for routine care during clinical trials
- Medical care at a federally qualified health center
- Tests and X-rays at a laboratory
- Care from a nurse midwife
- Medical care from certified pediatric and family nurse practitioners
- Services at a birthing center recognized by the state
- Help with transportation to medical appointments
- Counseling to help pregnant people stop smoking
Examples of Optional Medicaid Benefits
These include:
- Medicines prescribed by a doctor
- Visits to a clinic for medical care
- Therapy to help with physical movement
- Therapy to help with daily tasks
- Treatment for speech, hearing, and language problems
- Help with breathing problems
- Other services to diagnose, screen, prevent, or help recover from health issues
- Care for foot problems
- Eye check-ups and glasses
- Dental check-ups and treatments
- Artificial teeth
- Artificial body parts
- Glasses to help with vision
- Treatment from a chiropractor
- Visits to other medical professionals
- Special nursing care at home
- Staying in a facility for mental health treatment if you’re 65 or older
- Treatment in a facility for people with intellectual disabilities
- Services to help you at home and in the community under Section 1915(i)
- Personal assistance services that you can control yourself under Section 1915(j)
- Choosing community-based services first under Section 1915(k)
- Treatment for tuberculosis (TB)
- Staying in a hospital for mental health care if you’re under 21
- Health Homes program for people with ongoing health problems under Section 1945 of the Social Security Act
Telehealth Services
- Federal laws and regulations governing Medicaid generally do not offer explicit guidance on telehealth delivery methods or the standards for implementing telehealth.
- States possess significant leeway in determining coverage and reimbursement for their services provided through telehealth.
- States can incorporate telehealth services into their Medicaid programs through approved state plan amendments (SPAs).
- States are obligated to integrate telehealth delivery for certain benefits as stipulated by law or regulation, such as the Community First Choice Option under 1915(k).
In Summary
Medicaid and CHIP programs provide medical assistance to low-income individuals and families, with each state having its eligibility criteria and benefits. The Federal Medicaid Administration sets rules for Medicaid nationwide, while states manage their plans with oversight from the Centers for Medicare and Medicaid Services (CMS).
Eligibility for Medicaid is determined based on income, household size, and other factors, with Modified Adjusted Gross Income (MAGI) serving as a key consideration. It covers mandatory and optional benefits, including COVID-19 treatments until September 30, 2024.
DISCLAIMER: Please verify the information provided here with the primary source to ensure accuracy. We strive to present information correctly. It is advisable to confirm details directly from the primary source for accuracy and reliability.