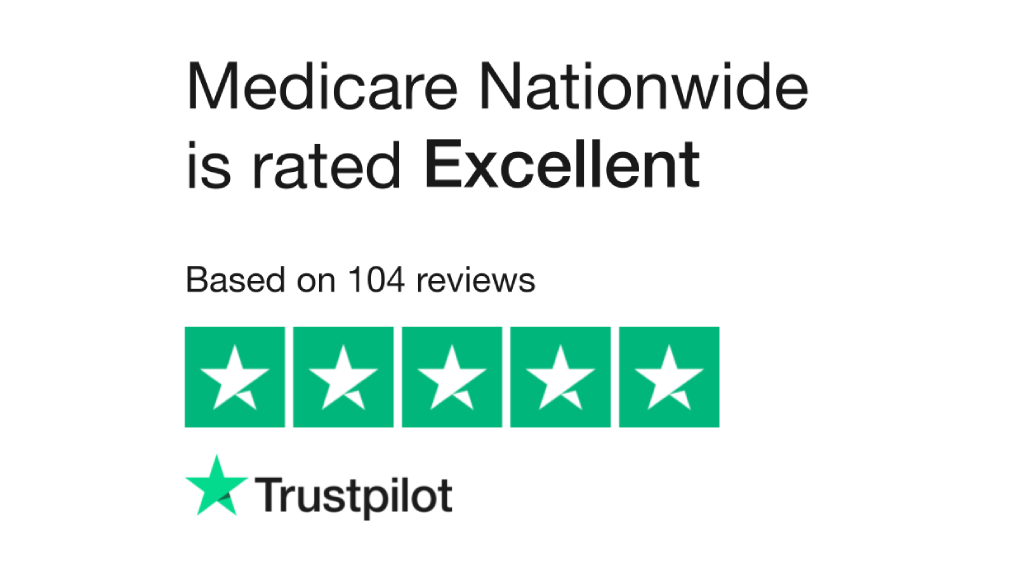
Families First Coronavirus Response Act (FFCRA)
Enrollment in Medicaid and Children’s Health Insurance Program (CHIP) increased from 70.7 million in Feb 2020 to 92.3 million in Dec 2022.
Resuming Eligibility and Enrollment Processes (Unwinding)
- In compliance with the Consolidated Appropriations Act (CAA), states are handling renewals for Medicaid and CHIP coverage.
- Some beneficiaries will undergo coverage renewal for the first time since the Public Health Emergency (PHE) began.
- The Centers for Medicare and Medicaid Services (CMS) collaborates with states and stakeholders to ensure eligible beneficiaries maintain coverage and facilitate transitions for those eligible for other forms of coverage.
- CMS approaches this task in two phases:
- Phase 1 involves informing beneficiaries about the renewal process and urging them to update their contact details.
- Phase 2 focuses on assisting Medicaid and CHIP beneficiaries with renewing their coverage and transitioning to alternative coverage if they no longer qualify for Medicaid or CHIP.
Partner Messages
- Partners can advise Medicaid and CHIP beneficiaries to get ready for renewing their coverage and explore other available health coverage alternatives.
- The primary messages partners should emphasize when communicating with individuals enrolled in it include:
- Keep your contact details current – Ensure your state possesses your accurate mailing address, phone number, email, or other contact details.
- Monitor your mail – Your state will send you a letter concerning your Medicaid or CHIP coverage.
- Complete your renewal form (if provided) – Fill out and promptly return the form to the state Medicaid or CHIP program to prevent any gaps in your coverage.
- If you are no longer eligible, there are alternative health coverage options – Take action promptly, as there are time constraints for enrollment. Visit HealthCare.gov/medicaid-chip/transfer-to-marketplace and Medicare.gov/sign-up-change-plans/joining-a-health-or-drug-plan/special-circumstances-special-enrollment-periods.
- Stay updated on messaging and resources by checking Medicaid.gov/Unwinding regularly.
Steps to Get Alternative Coverage
If your Medicaid or CHIP coverage is no longer applicable, there are alternative coverage options available to you. You might be eligible for a Special Enrollment Period (SEP) under the following circumstances:
- Marketplace: If you lost Medicaid or CHIP coverage within the past 60 days or anticipate losing coverage within the next 60 days.
- Medicare: If you are currently eligible but did not enroll when you first became eligible, your SEP extends for 6 months following the termination of its coverage.
If you are enrolled in both Medicare and Medicaid and lose your Medicaid coverage, your SEP extends for 3 months after receiving notice of Medicaid termination.
- You can take advantage of this period to:
- Enroll in a Medicare Advantage Plan or a Medicare prescription drug plan.
- Switch your existing Medicare Advantage Plan or Medicare prescription drug plan.
Coverage of Mandatory Medicaid Benefits for COVID-19 Treatments
Medicaid will continue to cover COVID-19 vaccines and treatments until September 30, 2024, with no additional expenses. After that date, coverage and associated costs may vary from state to state.
People enrolled in it can receive vaccines endorsed by the Advisory Committee on Immunization Practices (ACIP), including the COVID-19 vaccine, without any out-of-pocket expenses. Providers have the option to seek reimbursement for administering the COVID-19 vaccine to underinsured individuals through the COVID-19 Coverage Assistance Fund.
Enhancing Adult Vaccine Accessibility Through Medicaid & CHIP
- State Medicaid and CHIP programs must offer coverage for approved adult vaccines as recommended by the ACIP, including their administration, with no out-of-pocket costs.
- The individuals required to receive this coverage include:
- Most of its beneficiaries are classified as Categorically Needy;
- All of its beneficiaries are classified as Medically Needy; and
- CHIP beneficiaries aged 19 or older (including pregnant and postpartum individuals covered by CHIP).
- Effective Date: October 1, 2023 (commencing on the first day of the initial fiscal quarter occurring one year after enactment).
Medicaid Drug Utilization Review (DUR) Program
Activities and procedures within the DUR program aimed at addressing opioid use may involve:
- Imposing restrictions on the quantity of opioids prescribed
- Monitoring patients who use opioids concurrently with benzodiazepines
- Implementing requirements related to Prescription Drug Monitoring Programs (PDMP)
- Employing tools to assess daily morphine milligram equivalents
Dealing With Mental Health & Substance Use Disorders (SUDs)
The ultimate rule on mental health and SUD parity:
- Enhances accessibility to benefits for mental health and SUD.
- Mandates states to divulge information regarding mental health and SUD benefits.
- Mandates states to clarify reasons for denying any mental health or SUD service.
CMS and federal partners collaborate with states to enhance Medicaid services for individuals with SUDs or mental health issues via:
- Health Homes
- Certified Community Behavioral Health Centers
- Section 1115 Substance Use Disorder (SUD) demonstrations
Understanding Medicare-Medicaid Enrollees
Nationally, there are approximately 12.3 million individuals referred to as “dual eligibles.” These include individuals with Medicare who receive full Medicaid benefits (referred to as full dual) and those who receive assistance with Medicare expenses (referred to as partial dual). Medicare Savings Programs assist in covering Medicare premiums and, in some cases, additional out-of-pocket expenses.
For those fully eligible for both Medicare and Medicaid, Medicare typically covers expenses first, followed by Medicaid for services covered by both programs.
What is Children’s Health Insurance Program (CHIP)?
CHIP provides healthcare coverage for children in families with incomes too high to qualify for Medicaid but too low to afford private insurance. Funding for it comes from both federal and state governments, and individual states manage it. More than 7 million children are enrolled already.
A health insurance initiative offering affordable coverage to children in households with incomes exceeding Medicaid thresholds but falling short of private insurance. They may also extend coverage to pregnant women in certain states.
Every state provides its coverage and collaborates with its respective Medicaid program. Applications can be submitted at any time, and if eligibility is met, coverage can commence immediately, regardless of the time of year.
CHIP Eligibility
To qualify for it, a child should be:
- Younger than 19
- Without insurance
- A citizen or meets immigration rules
- Living in the state
- Within the state’s income limit for CHIP, based on family earnings and any other state-defined rules in the CHIP plan.
NOTE: Each state may include its own CHIP requirements, but must adhere to federal standards, methods, and procedures for eligibility.
State Options for CHIP
States have the flexibility to structure their CHIP program in three different ways. These are:
- Medicaid Expansion (10 states, the District of Columbia, and 5 U.S. Territories)
- Separate CHIP ONLY (2 states)
- Both Medicaid expansion and separate CHIP (38 states)
What is a Basic Health Program (BHP)
Additional Health Coverage for Low-Income Individuals:
- BHPs offer optional health insurance for those with limited income who don’t qualify for Medicaid, CHIP, or other essential coverage.
- States can offer coverage to citizens with incomes ranging from 133% to 200% of the federal poverty level (FPL).
- Lawfully present non-citizens with incomes between 0% and 200% of the FPL, who are ineligible for Medicaid or CHIP due to immigration status, can also receive coverage.
Currently, only Minnesota and New York have implemented BHPs.
Eligibility for Non-Citizens in Medicaid & Children’s Health Insurance Program (CHIP)
Typically, individuals who are not U.S. citizens must have a recognized immigration status and meet additional eligibility criteria set by the state to qualify for Medicaid or CHIP benefits. For most eligible non-citizens who arrived in the U.S. after August 22, 1996, there is a mandatory 5-year waiting period before they can apply for these benefits.
However, there are exceptions to the waiting period rule, which include refugees, asylees, Compact of Free Association (COFA) migrants, and qualified non-citizens who are veterans, active duty service members, as well as their spouses and children.
Eligibility Criteria for Qualified Non-Citizens under the Compact of Free Association (COFA)
States and the District of Columbia are required to provide Medicaid coverage to COFA migrants if they meet the eligibility criteria outlined in the state plan.
NOTE: The extension of coverage for COFA migrants does not include distinct CHIP programs.
State’s Choice for Providing Coverage to Lawfully Residing Children and Pregnant Individuals
- Allows states to offer both benefits to legally residing children and pregnant individuals in the United States, including those within their initial 5 years of holding qualified non-citizen status.
- This provision pertains to pregnant individuals eligible for Medicaid and CHIP, children up to the age of 19 for CHIP, and children up to the age of 21 for Medicaid, who meet the eligibility criteria for these programs.
Handling of Emergency Medical Situations
- In specific situations, Medicaid covers the expenses for treating emergency medical conditions for non-citizens lacking adequate immigration status.
- Non-citizens must have an emergency medical condition and fulfill all state-specific Medicaid eligibility criteria, including income and residency requirements.
Important Things to Keep in Mind
- Both, Medicaid and CHIP, are collaborative programs between the federal government and states.
- States have the authority to broaden eligibility criteria for additional groups and income brackets and opt to include optional benefits.
- A single application can assess eligibility for Marketplace plans, and cost-saving options within the Marketplace, Medicaid, and CHIP.
- Certain individuals are eligible for both Medicare and Medicaid.
- Both offer eligibility options and emergency treatment provisions for non-citizens in some cases.
- Recent federal laws and budget allocations, responding to and concluding public health crises, influence various aspects of these programs.
In Summary
The Families First Coronavirus Response Act (FFCRA) requires states to resume renewing Medicaid and CHIP coverage after the Consolidated Appropriations Act (CAA). This process involves informing beneficiaries about renewal procedures and transitioning them to alternative coverage if they are not eligible for both.
The FFCRA also addresses COVID-19 treatment coverage, adult vaccine accessibility, the Medicaid Drug Utilization Review (DUR) Program, and mental health and substance use disorder (SUD) parity. Additionally, it highlights eligibility criteria, coverage options, and procedures for non-citizens, including COFA migrants. Finally, it emphasizes the importance of state flexibility, integrated care models, and recent legislative impacts on both programs.
DISCLAIMER: Please verify the information provided here with the primary source to ensure accuracy. We strive to present information correctly. It is advisable to confirm details directly from the primary source for accuracy and reliability.